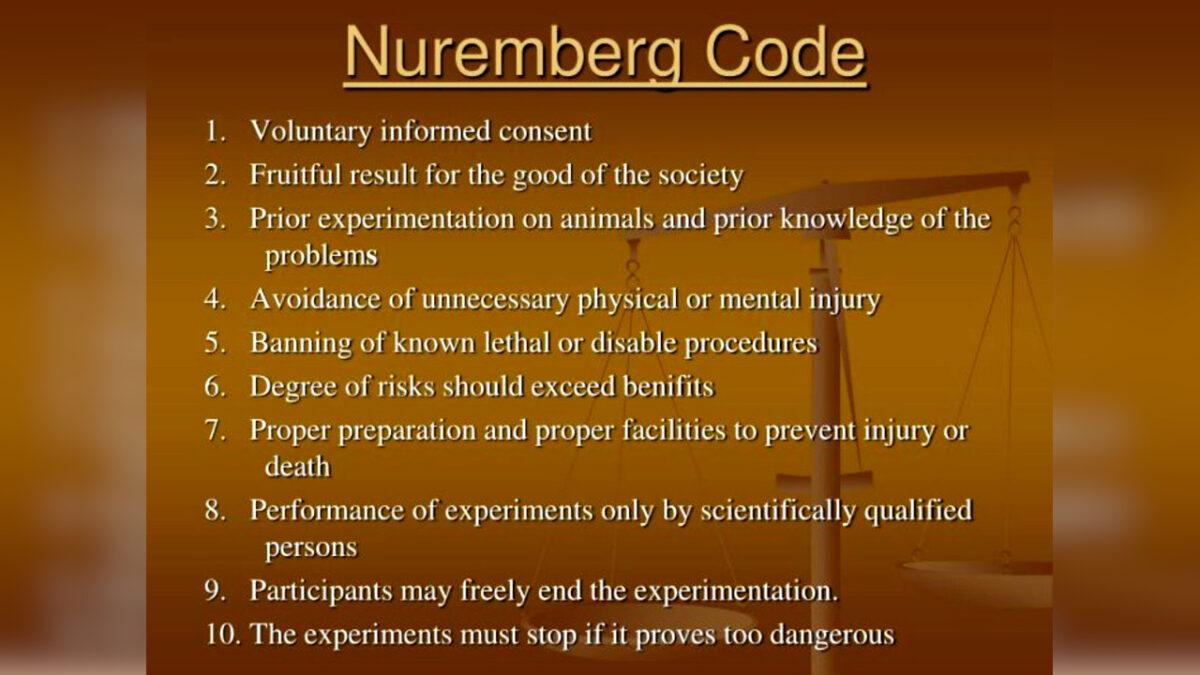
I’m not a lawyer, nor am I an “expert” in issues regarding standard of care, standard of medical practice, informed consent, and patient confidentiality. I do have 44 years of clinical experience in the military and in the private sector. While in the military and on deployment physicians and surgeons were required to have a working knowledge of the Nuremberg Code and The Helsinki Declaration. The Nuremburg Code of 1947 was established to ensure that informed consent was obtained prior to proceeding with any human experimentation or in clinical trials with patients:
The Nuremberg Code
The voluntary consent of the human subject is absolutely essential.
This means that the person involved should have legal capacity to give consent; should be so situated as to be able to exercise free power of choice, without the intervention of any element of force, fraud, deceit, duress, over-reaching, or other ulterior form of constraint or coercion; and should have sufficient knowledge and comprehension of the elements of the subject matter involved, as to enable him to make an understanding and enlightened decision.
The World Medical Association (WMA) of Helsinki 1964 extended the rights of all patients, not just those undergoing experimentation or clinical trials:
1. The World Medical Association (WMA) has developed the Declaration of Helsinki as a statement of ethical principles for medical research involving human subjects, including research on identifiable human material and data…
3. The Declaration of Geneva of the WMA binds the physician with the words, “The health of my patient will be my first consideration,” and the International Code of Medical Ethics declares that “A physician shall act in the patient’s best interest when providing medical care.”
4. It is the duty of the physician to promote and safeguard the health, well-being, and rights of patients, including those who participate in medical research. The physician’s knowledge and conscience are dedicated to the fulfilment of this duty.
There have been people who have tried to extrapolate the use of new mRNA vaccine technology as being experimental—including Dr. Robert Malone a virologist and researcher who helped develop the technology for the new mRNA technology. I am not an anti vaxer, and both my wife and I have received our vaccines and booster doses. All three times appropriate informed consent, and full disclosure as prescribed in both The Nuremburg and Helsinki were given to us. I do not believe that the vaccines are experimental and there was no coercion or infringement upon patient autonomy with me my wife and my family.
The issue of informed consent and patient autonomy and the applications of “Provider Standards of Care” in the clinical setting during the Covid surges needs to be reviewed. For me to try to formulate a legal opinion about these issues would be about as ludicrous and outlandish as a hospital administrator, or former Idaho Attorney General or the CEO of The IMA having a credible opinion about the validity of a scientific opinion that differs from the operative political agenda of the day. Especially when such people have credible medical credentials and expertise and can produce contemporary research and validation of their opinions. I can comment on the underlying moral principles involved without talking about THE LAW and the application of THE LAW. I can say that credible attorneys in several other states are looking at these issues and have used Nuremberg and Helsinki as guides for their arguments.
Around 2003 attempts were made to establish guidelines for declaring emergency procedures in mass triage situations involving trauma and pandemics. These efforts were passed onto the IMA and IHA and then to various hospitals throughout the State. Nobody could get along and petty jealousy and pridefulness resulted in the ball being kicked back to State agencies, who did truly little to establish CRISES STANDARDS OF CARE (CSC) until December of 2020. During the intervening 17 years a Board of Experts was established to guide and help set policy at The Idaho Department of Health and Welfare (DHW). This was part of the problem that put Idaho government behind the curve—look at Florida for example where their entire medical response mass casualty system was in place prior to the pandemic. The other problem was that the advisory board of experts had no public member, no practicing nurse, or no attorney on the board. Like Health South having an accounting department without any CPAs.
That same month December of 2020 the advisory Board hired a consulting firm from Salt Lake City for $40,000 to produce a template for an Idaho (CSC). Within days that plan was adopted as THE TEMPORARY RULE with the requirement that the plan would have to be reviewed and agreed upon by the legislature during the next session—Jan 2021. The DHW has adopted the Temporary Rule over 1 year ago and it is the rule now in effect without ever having been reviewed and approved by our legislature! As far as I can tell from reviewing legislative agenda logs no committee hearings have ever been scheduled and I cannot find where there has been a vote on the floor, and there has still been no public input regarding this rule. I would also like to know the involvement of either the Idaho Attorney General’s Office or outside council during this process. Prior to 2020 I can find attempts by the (DHW) to apply a matrix model to trauma but not to pandemics.
It is my understanding that early in the pandemic—before Dec. 2020, hospitals were writing protocols for patient care that would be deployed should a (CSC) be declared.
Who developed these protocols? Were these promulgated by the CDC or CMS? Did the hospitals ask the Governor or the (DHW) to initiate the (CSC)? Did they need such a declaration to initiate their protocols? Once a (CSC) is declared does that in any way limit the liability of providers—doctors and hospitals and with these protections do the clinical guidelines change? Are patients informed of these changes? Do the criteria of declaring a (DNR) change in patient resuscitation orders change? In New York State specific (CSC) guidelines were not established, but the legislature did vote to indemnify government agencies, the governor, and providers from liability during the first surge of the pandemic. That is why no one was held accountable for the 30,000 deaths that resulted from transferring sick Covid patients back to nursing homes where they infected other vulnerable patients. An act that had to have a doctor sign off on the transfer of the patient both at the transferring and receiving end. No legal accountability.
Are patients who refuse to be intubated or not agree to be treated under the terms of the clinical guidelines treated differently than those who do agree? Are they placed under a lower level of care and made DNR—do not resuscitate, sooner? I do not know. Do reimbursements change under a (CSC) order or when clinical protocols are deployed? What about when they aren’t deployed does reimbursement or access to Covid funds change?
Are living will documents honored the same way under the standards and guidelines? Are family members consulted and are they still required to be part of the decision-making process when guidelines and protocols are in place?
I believe everything that has been done up until now has been under the authority of a “temporary order.” The legality of not having the legislature pass a permanent rule needs to be explained. I am not able to discern nor am I in a position of the Idaho (AG) regarding the legality of what has gone on up until now. The spirit of Nuremberg and Helsinki has not been respected and in most cases not considered by the” experts.” The makeup of the (DHW) Board was such that these questions were not asked. The makeup of the Governor’s advisory Board should have had clinicians and nurses on it that were not only concerned with the clinical nuts and bolts of the pandemic, but also with the process of triaging patients and respecting their rights and autonomy. The moral predicate for the temporary order I believe was purposefully omitted from the language in the order.
“A physician shall act in the patient’s best interest when providing medical care… “
“It is the DUTY of the physician to safeguard the health, wellbeing, and RIGHTS of the patient”


One reply on “Crisis Standards of Care too Many Questions Left Unanswered”
Correction by Author: The company retained by the DHW for the (CSC) contract was Coordinated Consulting Service an Oregon Company